Automated Electronic Specimen Tracking Central to Increase Quality and Patient Safety
The processing of tissue samples through the anatomical pathology laboratory has typically been a very manual process, due to its complex nature and the level of skill required to prepare and review tissue specimens. A patient’s anatomical pathology test request is often associated with several specimens, blocks and slides. The gross tissue description and pathologist review of multiple slides create the patient report, which then goes on to form the basis for diagnosis and treatment plans. One error at any step of this process can result in incorrect reporting, creating the potential for misdiagnosis and incorrect treatment.
However, while the work may be complex, the most common errors in the histology lab are often simple. For example, the accidental transposition of patient specimens, where a label is applied to the wrong sample, or where a label is misread due to illegible handwriting.
Lab staff take great care to ensure that such errors do not occur, or at least are quickly rectified when they do, but the manual tracking of samples through the anatomical pathology lab is a time-consuming process. It requires reconciliation of blocks and work lists, and the manual logging of each step and action taken on every specimen.
Over recent years, histology labs have also been dealing with an increase in volume and complexity of work due to an aging population, new cancer treatment protocols and the expansion of cancer screening programs. Increasingly, labs are looking for ways to improve workflow efficiency to absorb their increasing workload and reduce the risk of error.
Specimen tracking technology, which has been in use in the clinical laboratory for a number of years, has now become available for the more complex AP workflow. A fully electronic specimen tracking system enables labs to move towards a leaner, automated workflow, and at the same time improve patient safety by ensuring accurate sample identification throughout the entire laboratory workflow.
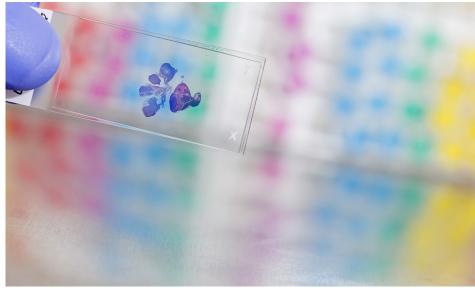
With a specimen tracking system, every item belonging to a patient case including blocks, cassettes and slides is uniquely identified using barcode labelling so that it can be traced at any point throughout the laboratory workflow. Only one patient request is processed at a time, eliminating the chance of accidental transposition of patients’ samples at the lab work bench.
As labs move away from batch-based and manual processing, including practices such as the pre-printing or hand-writing of labels, the opportunity for labelling errors is also greatly reduced. Instead, with single piece processing, cassette writers and slide printers are positioned at the appropriate points on the workbench. These are interfaced to the tracking system at each step so the correct number of legible, permanent labels are printed, just-in-time.
For example, at the specimen preparation stage, the barcode on the specimen pot is scanned, and the appropriate number of cassettes for the specimen type are automatically printed right then and there, with the unique case and specimen details embedded into the barcode. At the cutting stage, the barcoded cassette is scanned, triggering the slide writer to print the appropriate number of slides, uniquely labelled for the procedures / stains to be performed
When it comes to staining, information is retrieved from the system via an autostainer interface, directing the instrument as to the type of staining to perform, removing the need for manual staining work lists and setup in the staining instrument.
Introducing this type of technology also offers labs the opportunity to improve ergonomics at the workbench. With an automated, barcode driven workflow, printed worklists are no longer required. Instead, these are replaced by barcode scanners and wall-mountable touch screens at each step, saving valuable space at the work bench.
With the addition of request form imaging the lab can go completely paperless, as the scanned request form is available in the system for everyone to view, at any point in the process.
With a single source for specimen traceability it is easier to check up on progress of a particular patient request or locate a specimen if further lab work is required. In addition, an audit trail of all user activity makes it easier and quicker to meet accreditation requirements.
When choosing and implementing an automated electronic specimen tracking system there are a number of things to consider, both in terms of technology and impact on staff.
New hardware investments will be required, including touch screen computers, barcode readers, and slide or label printers as well as cassette writer instruments. However, some tracking systems may only work with particular instrument makes and models. More flexible systems can be interfaced to different auto strainers, cassette writers and slide printers so that the lab doesn’t get locked into using particular instruments.
In addition, there may be costs associated with developing an interface between the specimen tracking software and the LIS, unless it is a fully integrated system.
The introduction of an automated tracking system and single piece processing will likely result in considerable processing changes with implications for staff functions, so it is important to conduct a workflow analysis to assess the likely impact. While most labs report that overall turn-around time for sample processing is maintained or reduced, some processes may in fact become more time-consuming (at least initially while the new system is bedding-in) and some staff may end up with new responsibilities. When staff are already busy with their day-to-day jobs and are facing the prospect of a change to their role, they can often be resistant to the introduction of a new system. In these cases, it often helps to obtain their buy-in to the quality and patient safety objectives for the new system at the outset and continue to keep them informed and involved throughout the process.
While anatomical pathology labs using automated electronic tracking, technology are still in the minority, it is a technology whose time has come, and labs that go down this path say they wouldn’t go back.
References:
AP tracking: an eagle eye on blocks and slides: by Anne Paxton; CAP TODAY online; 2013
Efficiency and patient safety behind lab’s decision to implement specimen tracking system: Sysmex New Zealand; 2015
Errors in the pathology laboratory: Lopes M. Beatriz S; Journal of Neurosurgery; 2015
The Henry Ford Production System: reduction of surgical pathology in-process misidentification defects by bar code-specified work process standardization: Zarbo RJ, Tuthill JM, D’Angelo R, Varney R, Mahar B, Neuman C, et al; Am J Clin Pathol 131:468–477; 2009
Written by: Caroline Eddy
Caroline Eddy is a Marketing Communication Specialist at Sysmex.
